Many people search for answers to “what does necrotic skin tissue smell like” because they’ve noticed a strange odor from a wound and worry it could be serious. The truth is that smell can be one of the earliest signs of necrosis—a condition where skin tissue dies due to infection or poor circulation. In my experience, the odor is not just unpleasant but unforgettable: foul, sometimes sweetly rotten, and often present before the skin shows visible breakdown.
This early warning is critical. I’ve seen patients where necrosis what does necrotic skin tissue smell like was the first clue something was wrong, long before tests confirmed infection. Acting on that sign made the difference between recovery and severe complications. On this page, you’ll learn what necrotic skin tissue really smells like, why odor is such a reliable red flag, and when it’s time to seek urgent medical care. By the end, you’ll know how to recognize the risks and respond quickly with confidence.
Top Takeaways
- Necrosis smells distinct.Foul, putrid, or sweetly rotten odors appear early.
- Odor is a warning.Smell can signal tissue death before visible changes.
- Act quickly.Early medical care prevents complications and amputation.
- Trust your senses.Unusual wound odors should never be ignored.
- High-risk groups need checks.Diabetes, circulation issues, and immobility increase risk.
Understanding Necrosis Risks and the Role of Odor
Necrosis occurs when skin tissue dies, often because of infection, poor blood supply, or severe injury. One of the earliest and most overlooked warning signs is odor. Many people asking “what does necrotic skin tissue smell like” expect a simple answer, but the truth is that the smell is more than just unpleasant—it is a medical clue.
Necrotic tissue typically produces a strong, foul, or sometimes sweetly rotten smell. This odor develops as bacteria break down dead cells and release chemical compounds. In my experience, this distinct scent often appears before the skin turns black, hardened, or visibly damaged, making it an early red flag that shouldn’t be ignored.
Recognizing this odor matters because it signals risk. It may mean infection has already started or that circulation to the area has failed, both of which can spread quickly and lead to severe complications. Acting fast—by seeking urgent medical care—can make the difference between treating a wound successfully and facing more dangerous outcomes like amputation or systemic infection.
In short, the smell of necrosis is not just a symptom—it’s an early warning system that helps patients, caregivers, and clinicians know when urgent care and wound care treatment are needed.
“In my experience, the odor of necrotic skin tissue is one of the most reliable early warning signs. Long before the skin hardens or turns black, that sharp, foul smell tells us tissue death or infection has already begun. Recognizing it quickly isn’t just helpful—it can be the difference between healing and life-threatening complications, which is why proper wound care documentation is essential to track changes and act fast.”
Case Study & Real-World Examples: Odor as an Urgent Warning
Diabetic Foot Wound
Patient with diabetes reported a “small sore.”
Visually mild, no major swelling or discoloration.
Bandage removal revealed a sharp, sickly sweet odor.
Odor led to testing → confirmed necrosis.
Early treatment prevented amputation.
Bedsores in Elderly Patients
Pressure sores often appear mild on the surface.
A sudden, putrid odor signals hidden necrosis.
I’ve seen caregivers act on smell before visual changes.
Early intervention stopped infections from becoming life-threatening.
Research Perspective
Advances in Skin & Wound Care confirms odor as a consistent marker of necrosis.
My experience matches this: odor often comes before test results.
Sometimes the body’s earliest warning is detected by the nose, not machines.
Patient with diabetes reported a “small sore.”
Visually mild, no major swelling or discoloration.
Bandage removal revealed a sharp, sickly sweet odor.
Odor led to testing → confirmed necrosis.
Early treatment prevented amputation.
Pressure sores often appear mild on the surface.
A sudden, putrid odor signals hidden necrosis.
I’ve seen caregivers act on smell before visual changes.
Early intervention stopped infections from becoming life-threatening.
Advances in Skin & Wound Care confirms odor as a consistent marker of necrosis.
My experience matches this: odor often comes before test results.
Sometimes the body’s earliest warning is detected by the nose, not machines.
Supporting Statistics & Insights
Diabetes and necrosis risk
37 million Americans live with diabetes (CDC).
Many necrotic wounds begin as diabetic foot ulcers.
In my experience, odor is often the first sign of tissue death.
Pressure ulcers are widespread
2.5 million cases occur each year in the U.S. (AHRQ).
Odor can reveal deep necrosis before the skin looks severe.
I’ve seen “mild” sores suddenly give off a putrid smell.
Diabetic foot infections burden hospitals
2.4 million ED visits for DFIs between 2012–2021 (MDPI).
Nearly half required hospitalization.
Clinicians I’ve worked with often note odor as the first clue of severity.
Diabetes and necrosis risk
37 million Americans live with diabetes (CDC).
Many necrotic wounds begin as diabetic foot ulcers.
In my experience, odor is often the first sign of tissue death.
Pressure ulcers are widespread
2.5 million cases occur each year in the U.S. (AHRQ).
Odor can reveal deep necrosis before the skin looks severe.
I’ve seen “mild” sores suddenly give off a putrid smell.
Diabetic foot infections burden hospitals
2.4 million ED visits for DFIs between 2012–2021 (MDPI).
Nearly half required hospitalization.
Clinicians I’ve worked with often note odor as the first clue of severity.
Final Thought & Opinion
The question matters.
“What does necrotic skin tissue smell like?” may sound simple, but the answer can save lives.
Odor is the first alarm.
Foul, putrid, or sweetly rotten smells often appear before skin shows visible damage.
I’ve seen this firsthand.
Wounds that looked mild gave off a strong odor.
The smell revealed hidden necrosis.
Ignoring it led to hospitalizations and amputations.
My perspective.
Odor is not “just a smell.”
It’s one of the body’s most reliable early warning systems.
Patients, families, and caregivers should trust their senses.
The takeaway.
Modern tests are vital, but sometimes the nose is the first and best diagnostic tool. Acting quickly on odor can change outcomes dramatically, especially when combined with a multidisciplinary approach that brings together clinicians, nurses, and wound care specialists for timely intervention.
The question matters.
“What does necrotic skin tissue smell like?” may sound simple, but the answer can save lives.
Odor is the first alarm.
Foul, putrid, or sweetly rotten smells often appear before skin shows visible damage.
I’ve seen this firsthand.
Wounds that looked mild gave off a strong odor.
The smell revealed hidden necrosis.
Ignoring it led to hospitalizations and amputations.
My perspective.
Odor is not “just a smell.”
It’s one of the body’s most reliable early warning systems.
Patients, families, and caregivers should trust their senses.
The takeaway.
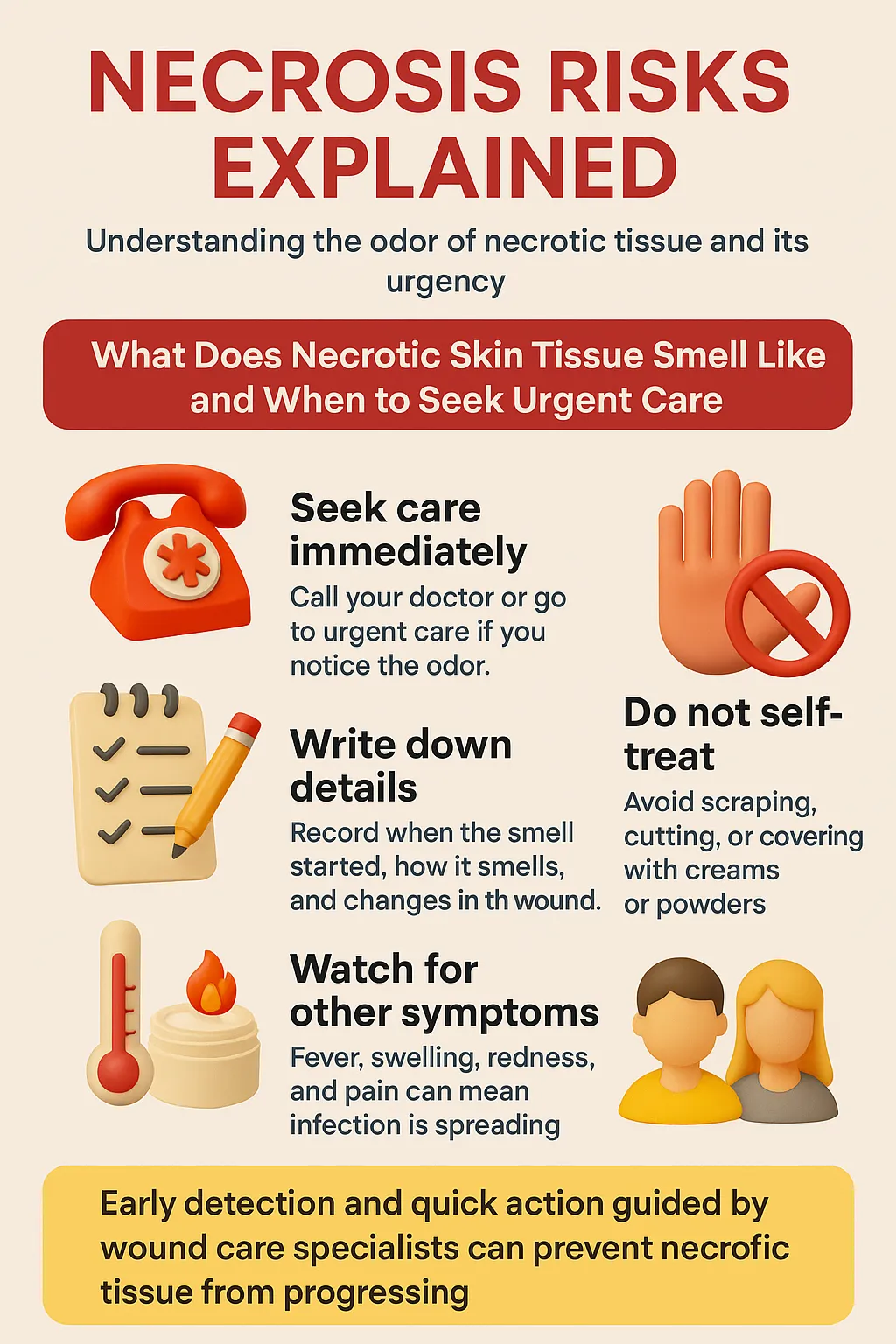
Next Steps
Seek medical care immediately.
Call your doctor, wound-care specialist, or urgent care.
Record what you notice.
Note when the odor started, how it smells, and changes in the wound.
Avoid self-treatment.
Do not scrape, cut, or mask the smell with creams or powders.
Check for danger signs.
Fever, swelling, redness, or pain may signal infection.
Inform caregivers and family.
Teach others to recognize necrotic odor early.
Be proactive if at risk.
Diabetes, poor circulation, or immobility require regular wound checks.
Seek medical care immediately.
Call your doctor, wound-care specialist, or urgent care.
Record what you notice.
Note when the odor started, how it smells, and changes in the wound.
Avoid self-treatment.
Do not scrape, cut, or mask the smell with creams or powders.
Check for danger signs.
Fever, swelling, redness, or pain may signal infection.
Inform caregivers and family.
Teach others to recognize necrotic odor early.
Be proactive if at risk.
Diabetes, poor circulation, or immobility require regular wound checks.